Men vs. Women: Who Really Feels More Pain
04/09/2024
Why Your Values Matter: A Personal Reflection on Filotimo
18/09/2024Unseen Agony: The Truth About Phantom Limb Pain
Understanding Phantom Limb Pain (PLP)
Have you ever heard of someone feeling pain in a body part that isn’t there anymore? It might sound impossible, but it’s a real thing called phantom limb pain. This happens when someone feels sensations, often painful ones, in a limb that has been amputated, either because of an accident or surgery. Let’s explore how this happens and why it’s such a strange, yet fascinating, part of how our bodies and brains work.
What is Phantom Limb Pain?
Phantom limb pain happens when someone who has lost a limb, like an arm or leg, feels pain, tingling, or itching in the limb that’s no longer there. Even though the limb is gone, the brain still thinks it’s there. For some people, this pain is mild, but for others, it can be very strong and affect their daily life.
Why Does It Happen?
To understand phantom limb pain, we need to look at how the brain and nervous system work. After a limb is amputated, the nerves that were connected to it are still in the remaining part of the body, like the stump. These nerves might keep sending signals to the brain, even though the limb is gone.
The brain has a “map” of the whole body, including the missing limb. When it gets these signals, it might get confused and act like the limb is still there, causing the feeling of pain.
As well as Phantom Limb Pain, people who have had an amputation might also feel something called phantom sensation, which is different from phantom limb pain. Phantom sensation is very common and doesn’t always mean the person feels pain.
There are three types of phantom sensations:
- Kinetic: Feeling like the missing limb is moving.
- Kinaesthetic: Sensing the size, shape, or position of the missing limb.
- Exteroceptive: Feeling touch, pressure, temperature, itch, or vibration in the missing limb. People may say “it feels like ants are crawling on my leg” when they don’t have a leg.
But let’s just concentrate on pain today.
The Brain’s Role in Phantom Limb Pain
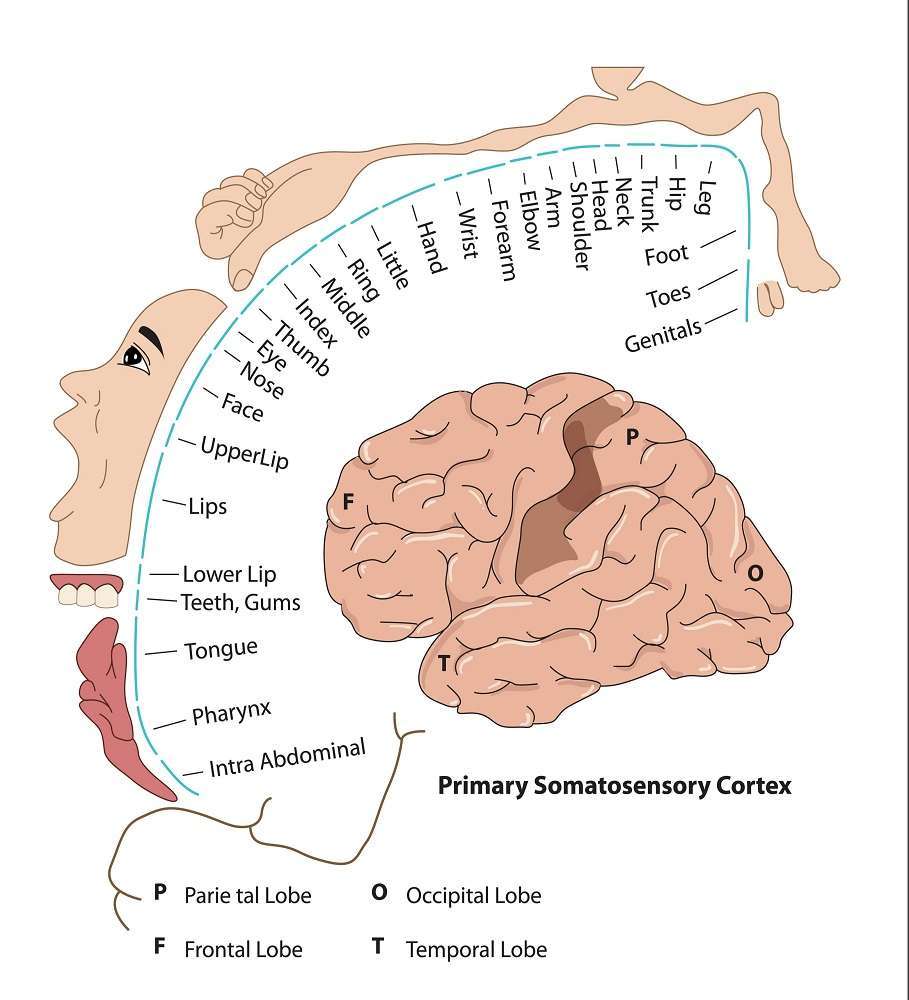
The brain plays a big role in phantom limb pain. Inside our brain, there’s a part called the somatosensory cortex. This area handles sensory information, like touch and pain, from different parts of our body. Even after a limb is gone, the part of the brain that was responsible for that limb is still there and active. This can confuse the brain, making it create the feeling of pain in the missing limb.
It’s almost like the brain is searching for the limb and, when it can’t find it, it sends out a “pain” signal instead. This is why phantom limb pain is often seen as a neurological issue, not just a physical one.
Theories on Phantom Limb Pain
Scientists are still trying to understand why phantom limb pain happens, but there are a few main ideas:
- Nerve Signal Mismatch: After an amputation, the nerves that are left might send confusing signals to the brain, which the brain interprets as pain.
- Rewiring of the Brain: The brain might try to reorganize itself after losing a limb, moving the “map” of the missing limb to nearby areas in the brain. This can cause mixed-up signals, leading to phantom pain.
- Psychological Factors: Emotions like anxiety or stress can make phantom limb pain worse, showing that both the mind and body are involved in this condition.
What are some causes and treatments of Phantom Limb Pain?
Phantom Limb Pain is complex and can be caused by a variety of factors—ranging from changes in the brain, sensitive nerves, emotional distress, or problems with muscles and joints. By understanding what’s causing the pain, treatment can be more targeted and effective, offering relief for those living with PLP.
Central Adaptation
When someone loses a limb, the brain adapts by reorganizing itself. This is called central adaptation. The brain keeps a “map” of the missing limb and may shift control to other areas, like the mouth or face, causing phantom limb pain. This can also happen with lower limb amputations, where control areas for organs like the bladder might move to the leg’s area, causing phantom pain.
- Treatment: Mirror therapy, sensory re-education, and brain stimulation techniques can help retrain the brain and reduce pain.

Peripheral Sensitisation
Peripheral sensitisation happens when the nerves in the remaining limb become overly sensitive, causing more pain. This occurs because the nervous system keeps sending pain signals, making it better at transmitting them. Stress, inflammation, or a poorly fitting prosthetic can worsen these signals.
Treatments include taking care of the limb, using medications, ensuring a good prosthetic fit, and practicing relaxation techniques to reduce stress.
- Treatment: Proper limb care, medications, ensuring a good prosthetic fit, and relaxation techniques to reduce stress.
Psychological and Social Factors
Stress, anxiety, and negative emotions can make Phantom Limb Pain (PLP) worse. Poor sleep and social problems can also contribute. When someone is stressed, the body releases a hormone called epinephrine, which makes nerves more sensitive and increases pain.
- Treatment: Mental health therapies like Cognitive Behavioural Therapy (CBT), Acceptance and Commitment Therapy (ACT), hypnotherapy, relaxation techniques, and improving sleep habits.
Musculoskeletal (MSK) Factors
Musculoskeletal issues involve problems with muscles and joints around the leftover limb. If these joints don’t work well or the muscles are weak, it can worsen Phantom Limb Pain. Doing exercises to keep joints flexible, strengthen muscles, and get ready for using a prosthetic can help reduce pain. A well-fitting prosthetic can also ease PLP by providing stability and making the remaining limb more useful.
- Treatment: Exercises to keep joints flexible, strengthen muscles, and prepare for prosthetic use. A well-fitting prosthetic can also provide stability and reduce pain.
Why is Phantom Limb Pain Important to Study?
Phantom limb pain helps us understand how the brain processes pain. It shows that pain isn’t always caused by injury or damage to the body; it can be created by the brain even when the body part is gone. This insight helps scientists and doctors understand chronic pain conditions that persist without a clear cause.
The Future of Phantom Limb Pain Research
As scientists study phantom limb pain, they find new ways to treat it and help people manage their pain. This research also reveals the brain’s amazing ability to change and adapt, which could lead to breakthroughs for many other types of pain.
Final Thoughts
Phantom limb pain is a fascinating example of how complex our brains and nervous systems are. Even though a limb is gone, the brain continues to feel it—and sometimes in painful ways. By learning more about this condition, we’re gaining insights into the mysteries of the brain, pain, and how to better treat people suffering from all kinds of chronic pain.
Technology plays a big role in treatments using Virtual Reality (VR) and Augmented Reality (AR). These tools can create a virtual limb for someone who has lost a limb, allowing them to see and move it in a 3D space, as if the limb is still there. This virtual limb can be used to interact with the world around them, helping with their therapy.
Another benefit of VR is that it can create virtual environments that are designed around the patient’s interests, making therapy more engaging and enjoyable. This helps patients stay motivated and get the most out of their treatment.[1]
Virtual Reality at Paragon PsychConnect
We are using VR in our work at Paragon PsychConnect allowing people with amputated limbs to walk around gardens, drive cars and many other activities allowing their brain to remap the amputated limb (an upgraded to the old mirror box therapy) and decrease pain.
[1] Rutledge T, Velez D, Depp C et al. A virtual reality intervention for the treatment of phantom limb pain: development and feasibility results. Pain Med. 2019;20(10):2051–2059